Most organizations are working to reduce stigma and empower employees to seek help for depression and anxiety. But just 20% of employers have done the same for addiction — even though 3 in 4 adults living with a substance use disorder are in the workforce.1,2 To fully support workforce health, businesses need to view addiction through the same lens as other mental and physical health conditions, and become recovery-ready.
Opioids, addiction, and creating a recovery-ready workplace


An equal-opportunity destroyer
The human cost of the opioid crisis is well documented. And one of the most powerful takeaways is that addiction doesn’t discriminate. There are people from every age group, ethnicity, tax bracket, education level, and industry who struggle with it. The problem is bigger than opioids — the underlying issue is that addiction is a serious disease, but only 1 in 10 people who need treatment ever get it.3
Addiction and substance misuse take a massive toll on the economy — over $442 billion per year.4 Businesses bear much of that burden through increased health care costs, absenteeism, and lost productivity. However, employers remain largely unaware of just how severely addiction is impacting their companies.

The impact of substance misuse on businesses
Health care costs are more than 3 times higher for employees who misuse any prescription pain medication — and up to 9 times higher for those who misuse opioids specifically.5,6 They’re more than twice as likely to be hospitalized — and their hospital stays are more than twice as long. These employees also miss a whopping 29 workdays a year — 3 times more than average.7
Many employees living with addiction and substance use disorders have co-occurring mental health conditions. For example, depression and anxiety are 4 times more common in people who misuse pain medication.8 Dependence on more than one substance is also common. Nearly 40% of people who misuse illicit or prescription drugs also misuse alcohol.9 The associated health risks for employees — and costs to employers — add up quickly.

Seeing the person behind the addiction
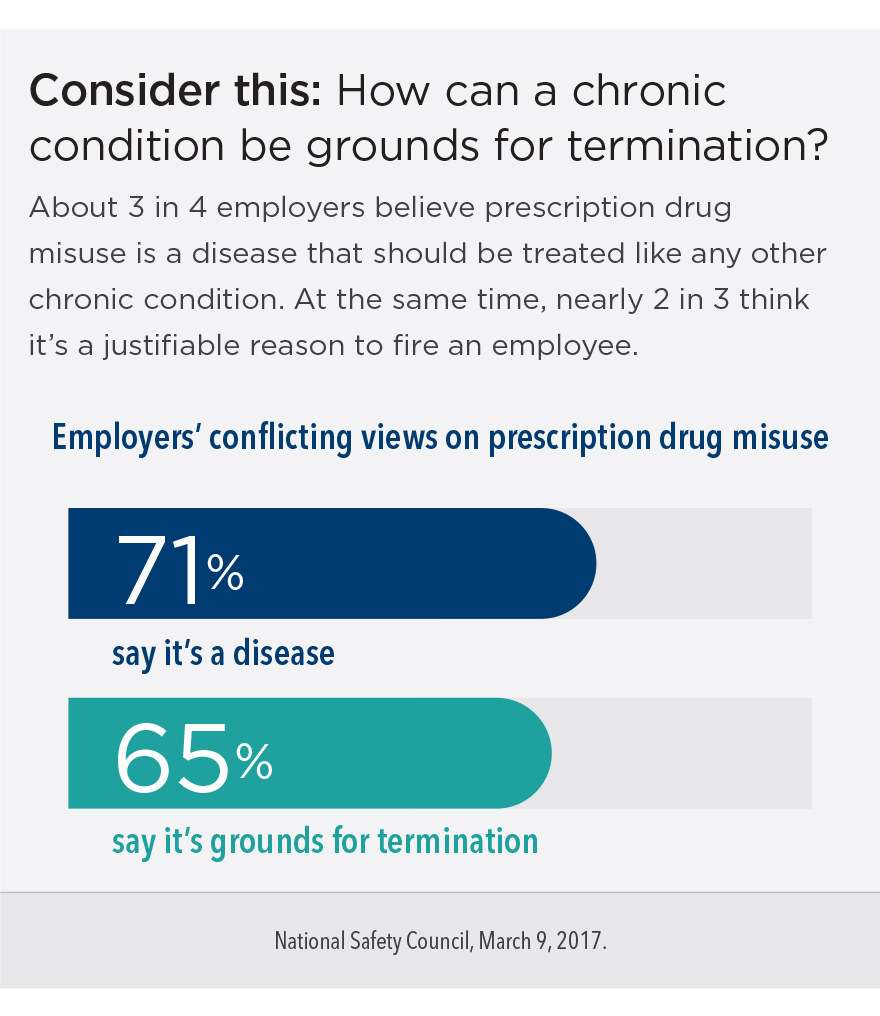
According to the American College of Physicians, addiction is a disease that can be treated and managed successfully — not unlike diabetes. But in most workplaces, it’s treated quite differently. Drug-free workforce policies typically focus on penalties — frequently resulting in termination — instead of helping employees get and stay healthy. Such policies may perpetuate the stigma and feelings of shame and fear that prevent so many people from seeking help.
It’s possible for high-performing employees who bring tremendous value to their organizations to also struggle with substance misuse or addiction. If they’re simply fired, these employees lose the income, routine, social support, and self-confidence they get from their job — along with health benefits that could have helped them access treatment. And on top of losing team members with institutional knowledge and experience, the employer spends 20% of each former employee’s annual salary to replace them.10 With 25% of employers struggling to find new recruits who are opioid-free, it’s time to explore a different approach.11
Recovery is good for business
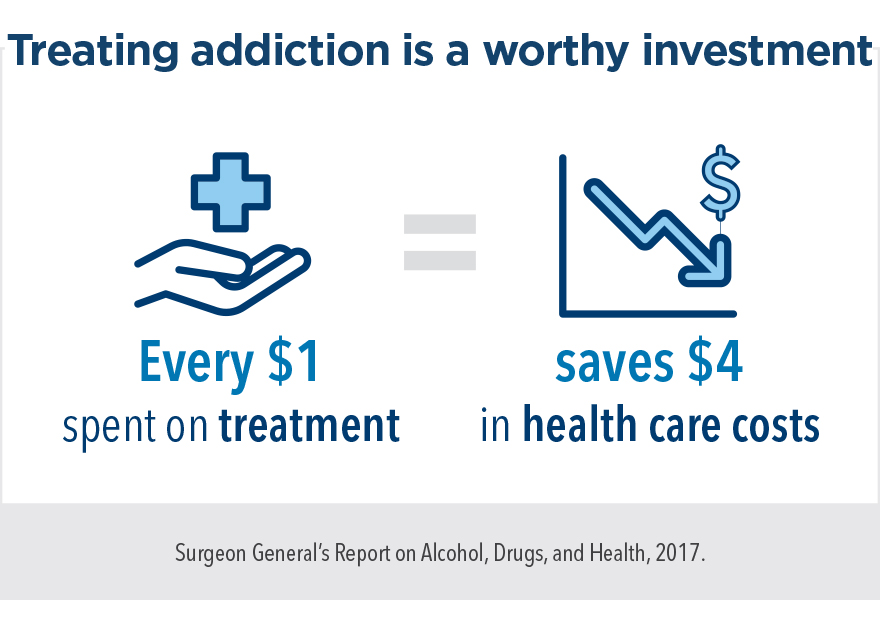
It’s true that treatment for addiction costs money. But every dollar a business spends helping employees get treatment saves $4 in health care costs.12 On average, each worker in recovery saves their employer $3,200 annually. For some industries, it’s more than $8,400.13
Investing in employee recovery benefits everyone. Recovery is a lifelong commitment that goes beyond rehabilitation, and it can transform a person personally and professionally. Workers in recovery tend to be model employees — extremely loyal and dependable, with fewer missed workdays and lower turnover rates than any other group.14
How to become a recovery-ready workplace
While prevention should be part of every workforce health strategy, support shouldn’t end there. In a workplace where treatment for addiction is encouraged rather than stigmatized, employees have better chances of recovery. It also sends a hopeful, positive message to all employees — and helps foster an inclusive work culture.
Take a stand against stigma
Stigma is one of the primary reasons why 90% of people who need treatment for addiction never get it.15 When people feel safe to talk openly and honestly about addiction and recovery, that stigma starts to break down. Just knowing that their employer views addiction as a treatable illness — and believes that recovery is possible — can empower employees to speak up and seek help.
Make recovery accessible
Employees need to know — and trust — that they can access treatment confidentially and without jeopardizing their jobs. Make sure your health plan covers all possible options, including behavioral therapy, addiction and recovery services, and medications like buprenorphine and naltrexone. Offer an employee assistance program (EAP) that can help employees navigate available resources.
Provide ongoing support
Some people continue working while they get treatment for addiction. Others need to take time off. Either way, it’s important to remember that treatment is just the first step. Creating a supportive work environment for recovering employees is just as important for long-term sobriety:
- Make reasonable accommodations, like flexibility to attend therapy during business hours.
- Consider making work events alcohol-free to be more inclusive of employees in recovery.
- Support a healthy work-life balance. Recovery requires time for self-care and social support, so employees need to know it’s OK to take breaks and time off.
To end this current crisis, attitudes about addiction need to change. We need to start seeing it for what it really is — a treatable health condition that people can and do recover from. As an employer, you can make a difference — because when businesses implement proactive, compassionate programs designed to break down stigma and connect employees to support, recovery happens.
Learn about Kaiser Permanente’s approach to mental health and addiction medicine >
About our expert

Paul Bryant is the Director of Kaiser Permanente’s Addiction Medicine Program in the Northwest. Paul has worked in the field since 2004 — treating adolescents struggling with addiction and co-occurring mental health issues, and overseeing adult services in outpatient, residential, and withdrawal management settings. In addition, Paul works with a cross-functional team of Kaiser Permanente providers to deliver one of the Northwest’s largest medication-assisted treatment programs.
Resources you may find helpful



- 1
The Employer Response to Opioids, National Business Group on Health, 2018.
- 2
Eric Goplerud et al., “A Substance Use Cost Calculator for US Employers with an Emphasis on Prescription Pain Medication Misuse,” Journal of Occupational and Environmental Medicine, November 2017.
- 3
Surgeon General’s Report on Alcohol, Drugs, and Health, U.S. Department of Health and Human Services, 2017.
- 4
See note 3.
- 5
See note 2.
- 6
“Implications of Drug and Alcohol Use for Employers,” National Safety Council, nsc.org, accessed January 3, 2020.
- 7
See note 2.
- 8
See note 2.
- 9
See note 2.
- 10
See note 2.
- 11
See note 1.
- 12
See note 3.
- 13
See note 2.
- 14
See note 2.
- 15
See note 3.
Kaiser Permanente health plans around the country: Kaiser Foundation Health Plan, Inc., in Northern and Southern California and Hawaii • Kaiser Foundation Health Plan of Colorado • Kaiser Foundation Health Plan of Georgia, Inc., Nine Piedmont Center, 3495 Piedmont Road NE, Atlanta, GA 30305 • Kaiser Foundation Health Plan of the Mid-Atlantic States, Inc., in Maryland, Virginia, and Washington, D.C., 2101 E. Jefferson St., Rockville, MD 20852 • Kaiser Foundation Health Plan of the Northwest, 500 NE Multnomah St., Suite 100, Portland, OR 97232 • Kaiser Foundation Health Plan of Washington or Kaiser Foundation Health Plan of Washington Options, Inc., 1300 SW 27th St., Renton, WA 98057
Congratulations! You have successfully saved this item.
To access your Saved items any time, open the "Saved Items" folder in the top right corner of the page.
It seems that you do not have cookies enabled. Please enable cookies to make use of all of our site's functionality.
You haven't collected any items yet.
- Save Content
Click the "Save" icon next to the content you want to revisit later.
- Access Your Saved Items
Click on the "Saved Items" link at the top of the page or use the URL we create for you.
Be sure to copy and paste the URL we create for you before you leave the site.
1-5 of 14
Your Link
After leave the site, your saved items will be saved for you at this URL:
https://business.preview.dpaprod.kpwpce.kp-aws-cloud.org/saved-items?user=Share your list
Show Disclaimer +


