About 75% of employees have struggled with an issue that affected their mental health.1 Yet, 8 out of 10 workers with a mental health condition say shame and stigma prevent them from seeking mental health care.2 That’s a problem for individuals, but it’s also a problem for employers — because untreated mental health conditions cost American companies billions every year. In fact, untreated depression costs $9,450 per employee, per year in absenteeism and lost productivity.3
Mental health in the workplace — and the cost of staying silent



What stigma looks like — and why it’s a problem
Mental health conditions are common and treatable. So why don’t we talk about them as openly as physical conditions like diabetes or asthma? Because of stigma — negative stereotypes about mental illness that persist both in and out of the workplace.
Though mental health conversations have increased in recent years, stigma remains a pervasive barrier in work environments. The majority of employers and employees report workplace stigma around mental health.4
Even in the most progressive workplaces, many employees keep their conditions secret. They may be afraid that being open about them will hurt their reputation, compromise work relationships, or even jeopardize their job. This can prevent employees from seeking help and getting better.
The cost of staying silent
Because stigma drives silence, employers simply can’t afford not to talk about this issue. The mental health of your workforce and your company’s bottom line are inextricably linked.
- Employees with untreated mental health conditions use nonpsychiatric health care services 3 times more than those who do get treatment.5
- Mental illness is the single greatest cause of worker disability worldwide.6
- 62% of missed workdays can be attributed to mental health conditions.7
- 50% of full-time employees have left a role for mental health reasons and the number is significantly higher for Millennials (68%) and Gen Zers (81%).8
- Mentally distressed workers are 3.5 times more likely to have substance use disorders.9


Prioritize mental well-being in the workplace
Learn how to prioritize your employees’ mental health and emotional well-being for a more present, productive, and invested workforce.
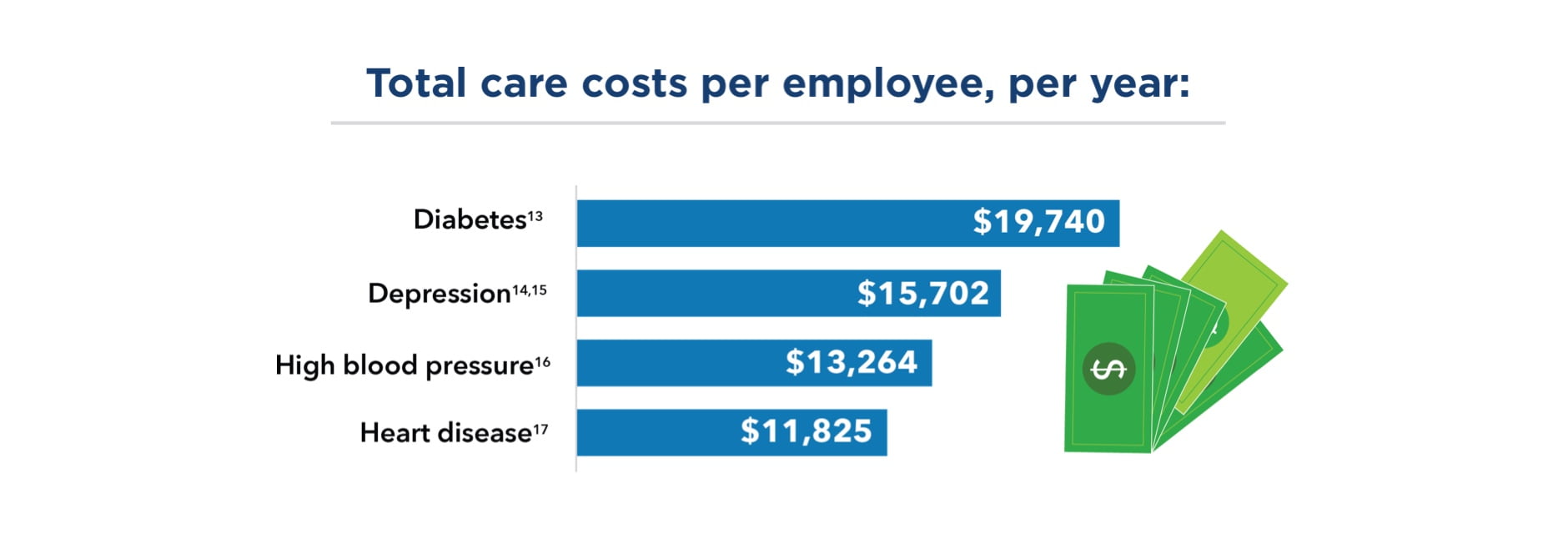
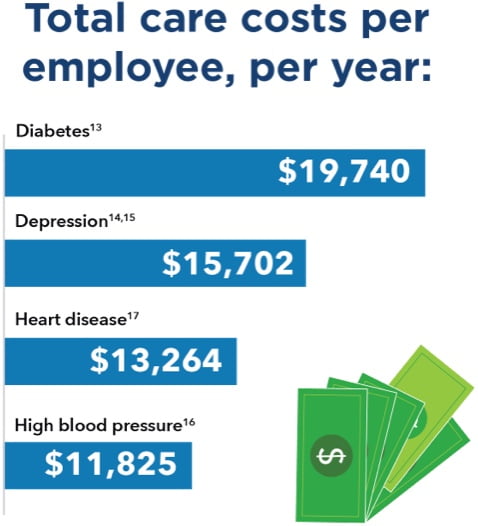
Compounding costs add up quickly
Mental health conditions are associated with the prevalence, progression, and outcome of certain physical conditions. Employees with untreated mental health conditions tend to have more serious and costly health issues in general. For example, their risk for heart attacks and strokes is twice as high — and cardiovascular disease is America’s most costly and prevalent chronic condition.10,11 And people with severe mental health issues are twice as likely to develop type 2 diabetes.12
Taking a stand against stigma
It’s clear that stigma is a significant barrier to mental health care, but it doesn’t have to be. And it shouldn’t be — because most people who get help get better. Depression is estimated to cause 200 million lost workdays each year.18 However, nearly 70% of people with a mental health condition or substance use disorder make a full recovery.19
To help more people get the care they need, it’s essential to understand stigma and take action to overcome it. Employers have an opportunity to address stigma head-on — to make sure employees feel supported, and to help set the tone for a productive and mentally healthy workforce.
About our expert

Don Mordecai, MD, is the Kaiser Permanente National Leader for Mental Health and Wellness. He’s been with Kaiser Permanente since 2003. Dr. Mordecai trained at Stanford University School of Medicine in child, adolescent, and adult psychiatry. His clinical work is with patients with developmental disorders, ADHD, and a range of general psychiatry issues. Dr. Mordecai also serves as adjunct clinical professor of psychiatry at Stanford University School of Medicine.
Resources you may find helpful



- 1
Mental Health: A Workforce Crisis,” American Heart Association CEO Roundtable, 2018.
- 2
“StigmaFree Company,” National Alliance on Mental Illness, NAMI.org, accessed January 31, 2019.
- 3
See note 1.
- 4
“National surveys reveal disconnect between employees and employers around mental health need”, McKinsey & Company, April 21, 2021.
- 5
“Bad for Business: The Business Case for Overcoming Stigma in the Workplace,” National Alliance on Mental Illness of Massachusetts, 2015.
- 6
See note 1.
- 7
See note 5.
- 8
Kelly Greenwood and Julia Anas, “It’s a New Era for Mental Health at Work,” Harvard Business Review, October 4, 2021.
- 9
“New Mental Health Cost Calculator Shows Why Investing in Mental Health is Good for Business,” National Safety Council, May 13, 2021.
- 10
Whiteman, “Mental illness linked to increased risk of heart disease, stroke,” Medical News Today, October 27, 2014.
- 11
Cardiovascular Disease: A Costly Burden for America,” American Heart Association, February 14, 2017.
- 12
Mangurian et al., “Diabetes and Prediabetes Prevalence by Race and Ethnicity Among People With Severe Mental Illness” Diabetes Care, June 2018.
- 13
Hugh Waters and Marlon Graf, “The Cost of Chronic Diseases in the U.S. Executive Summary,” Milken Institute, May 2018.
- 14
Garen Staglin, “Understanding the Evidence: Transforming How Employers Make the Case for Mental Health,” Forbes, April 4, 2019.
- 15
See note 1.
- 16
See note 13.
- 17
See note 13.
- 18
“Depression Evaluation Measures,” Centers for Disease Control and Prevention, accessed September 21, 2022.
- 19
“People Can Recover and Thrive After Mental Illness and Substance Use Disorders,” Association for Psychological Science, April 29, 2022.
Kaiser Permanente health plans around the country: Kaiser Foundation Health Plan, Inc., in Northern and Southern California and Hawaii • Kaiser Foundation Health Plan of Colorado • Kaiser Foundation Health Plan of Georgia, Inc., Nine Piedmont Center, 3495 Piedmont Road NE, Atlanta, GA 30305 • Kaiser Foundation Health Plan of the Mid-Atlantic States, Inc., in Maryland, Virginia, and Washington, D.C., 2101 E. Jefferson St., Rockville, MD 20852 • Kaiser Foundation Health Plan of the Northwest, 500 NE Multnomah St., Suite 100, Portland, OR 97232 • Kaiser Foundation Health Plan of Washington or Kaiser Foundation Health Plan of Washington Options, Inc., 1300 SW 27th St., Renton, WA 98057
Congratulations! You have successfully saved this item.
To access your Saved items any time, open the "Saved Items" folder in the top right corner of the page.
It seems that you do not have cookies enabled. Please enable cookies to make use of all of our site's functionality.
You haven't collected any items yet.
- Save Content
Click the "Save" icon next to the content you want to revisit later.
- Access Your Saved Items
Click on the "Saved Items" link at the top of the page or use the URL we create for you.
Be sure to copy and paste the URL we create for you before you leave the site.
1-5 of 14
Your Link
After leave the site, your saved items will be saved for you at this URL:
https://business.preview.dpaprod.kpwpce.kp-aws-cloud.org/saved-items?user=Share your list
Show Disclaimer +


